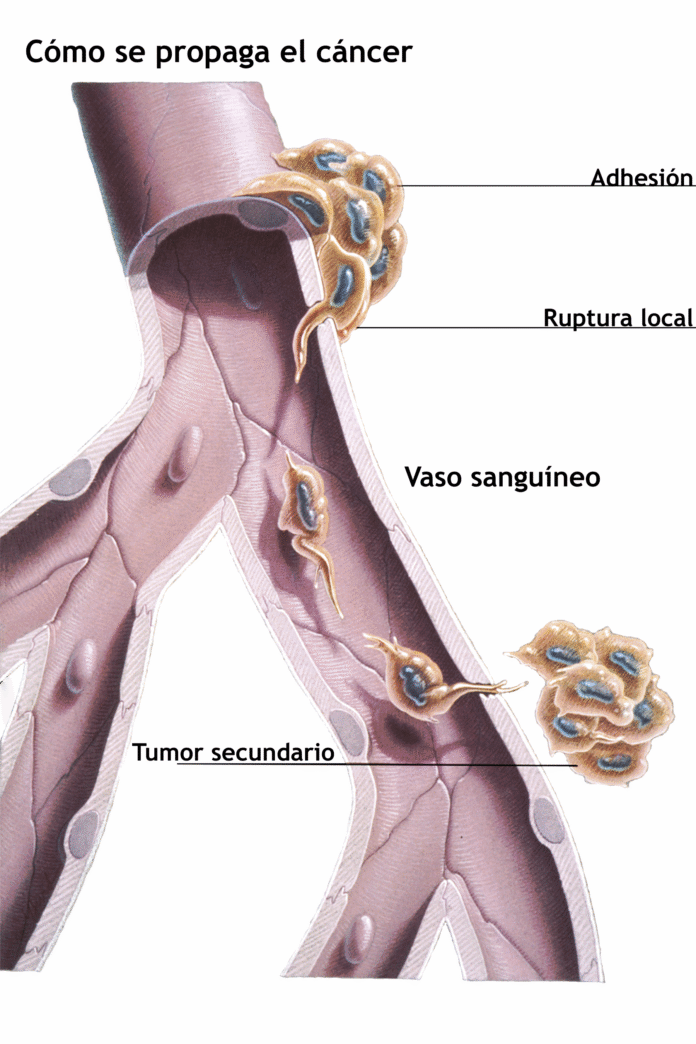
Metastasis—the process by which cancer spreads from its original site to other parts of the body—remains the leading cause of cancer-related mortality. Although decades of research have illuminated the genetic mutations that drive tumor initiation and growth, less is known about how a tumor’s genome evolves when it seeds new locations. A newly published study from Weill Cornell Medicine and Memorial Sloan Kettering Cancer Center (MSK) offers critical insights into this question, revealing that metastatic tumors accumulate large-scale chromosomal changes—known as copy-number alterations (CNAs)—far more frequently than simple point mutations. These findings, appearing June 2 in Nature Genetics, may reshape how clinicians predict metastatic progression, tailor targeted therapies, and deploy immunotherapy in advanced cancers.
Study Design and Scope: A Comprehensive Genomic Comparison
Large Patient Cohort and Multiple Cancer Types
Researchers led by Dr. Luc Morris (MSK), Dr. Xi Kathy Zhou (Weill Cornell), and Dr. Chaitanya Bandlamudi (MSK) analyzed genomic data from more than 3,700 patients across 24 distinct cancer types. Crucially, each patient contributed paired samples: one from the primary tumor and one from a metastatic lesion biopsied at a later time. By leveraging MSK’s proprietary tumor sequencing platform—MSK-IMPACT—the team generated high-resolution profiles of somatic mutations, small insertions/deletions, and CNAs in both primary and metastatic tissues.
Longitudinal Sampling and High-Depth Sequencing
Most patients in the cohort had multiple biopsies over the course of their disease, enabling a dynamic view of tumor evolution. High-depth sequencing (mean coverage >500×) ensured reliable detection of subclonal alterations. The investigators then computationally compared each pair—primary versus metastatic—focusing on two categories of genomic change: (1) single nucleotide variants (SNVs) and small indels, collectively referred to as “mutations,” and (2) larger chromosomal gains or losses, designated copy-number alterations (CNAs).
Key Finding: Metastases Harbor Significantly More CNAs than Mutation
Overall Enrichment of CNAs in Metastatic Samples
Across the entire cohort, metastatic tumors exhibited a marked increase in CNA burden relative to their matched primaries. Whereas the number of new point mutations acquired between diagnosis and metastasis was relatively modest, metastatic lesions frequently displayed widespread gains and losses of chromosomal segments—sometimes encompassing entire chromosome arms or whole chromosomes. Quantitatively, the median CNA burden (measured in megabases of altered DNA) in metastases was more than double that of primary tumors.
Whole-Genome Doubling as a Hallmark Event
One striking observation was the prevalence of whole-genome doubling (WGD)—the duplication of an entire set of chromosomes—in nearly one-third of metastatic samples. In contrast, WGD occurred in only about 10–12% of primary tumors. WGD was most common in cancers of the breast, lung, and prostate, but it was also observed in colorectal, pancreatic, and melanoma metastases. Importantly, WGD serves as an extreme CNA: by doubling the entire genome, cancer cells can buffer deleterious mutations and tolerate large-scale gene amplifications or deletions.
Relative Stability of Point Mutation Accumulation
In contrast to the dramatic rise in CNAs, the number of new point mutations identified in metastases was modest. Although individual driver mutations—such as those in TP53, PIK3CA, or KRAS—were carried forward from the primary lesion, few entirely novel SNVs emerged as universal hallmarks of metastatic progression. Instead, the study suggests that while some additional mutations continue to accrue over time, the predominant genomic shift enabling metastatic fitness arises from large-scale structural alterations rather than from incremental point-mutational “tweaks.”
Biological Rationale: Why CNAs Dominate in Metastasis
CNA Versus Mutation: A Trade-Off Between Adaptive Potential and Immune Visibility
Mutations often generate neoantigens—novel peptides that can be recognized by the host immune system. Consequently, tumors burdened with high mutational load may be more susceptible to immune surveillance and, under selective pressure, must develop mechanisms of immune evasion. By contrast, copy-number alterations enable cancer cells to adapt through dosage changes of entire gene sets—upregulating oncogenic pathways or deleting tumor suppressors—without necessarily exposing new neoantigens.
Whole-Genome Doubling as an Adaptation Strategy
Whole-genome doubling gives metastatic cells an evolutionary advantage. By temporarily increasing ploidy from diploid to tetraploid, cells acquire additional gene copies that buffer essential cellular machinery. Duplications permit the silencing of tumor suppressor genes (for instance, via homozygous deletion of the remaining copy) while preserving a backup. This genomic “doubling” also facilitates rapid acquisition of further CNAs: subsequent gain or loss of single chromosomes or segments can occur on the tetraploid background with reduced lethality.
Clinical Correlation: CNA-High Tumors Are Where Immunotherapy Fails
Clinical data demonstrate that tumors with high CNA burdens often correlate with poor responses to immune checkpoint inhibitors, despite sometimes having moderate mutational burdens. This suggests that metastatic tumors, by accruing CNAs, gain a competitive edge against both targeted therapies (through gene amplification) and immunotherapy (by avoiding the generation of strong neoantigens).
Implications for Precision Oncology and Immunotherapy
Refining Biomarkers: Tumor Mutational Burden Versus CNA Score
Traditionally, tumor mutational burden (TMB) has been used to stratify patients for checkpoint blockade therapy (e.g., anti-PD-1, anti-PD-L1). However, the Weill Cornell/MSK study highlights that CNA burden—quantified as the fraction of the genome affected by copy-number gain or loss—may serve as an equally or more vital biomarker in the metastatic setting. Patients with high CNA scores but low TMB may fail immunotherapy, whereas those with low CNA scores might retain immunogenic mutations that render them better candidates. Future assays may thus need to integrate both TMB and genome-wide CNA profiling to personalize treatment.
Targeting CNA-Driven Pathways and DNA Repair Vulnerabilities
Metastatic cells that undergo whole-genome doubling and subsequent aneuploidization often exhibit heightened genomic instability and reliance on DNA repair mechanisms. Drugs targeting DNA-damage response pathways—such as PARP inhibitors—could be more effective against CNA-high tumors, especially those lacking homologous recombination proficiency. The study suggests exploring synthetic lethality strategies: for instance, combining cell-cycle checkpoint inhibitors with agents that induce replication stress to exploit the vulnerabilities of aneuploid metastatic cells.
Microenvironment Remodeling and Resistance
The observed genomic divergence between primary and metastatic lesions may also drive changes in the tumor microenvironment. Metastatic metastases frequently display increased stromal infiltration, altered cytokine profiles, and recruitment of immunosuppressive cell types (e.g., myeloid-derived suppressor cells). By understanding which CNAs correlate with particular microenvironmental shifts—such as MYC amplification promoting a neutrophil-rich infiltrate—clinicians could trial combined regimens that target both cancer-cell–intrinsic pathways and immunosuppressive niches.
Study Highlights and Notable Observations
1. Cohort Diversity and Robust Statistical Power
With over 3,700 patients spanning lung, breast, colorectal, prostate, pancreatic, melanoma, and other solid tumors, the study’s scope provides robust statistical confidence. The inclusion of paired timepoints—sometimes years apart—permits dissection of how individual tumors shift their genomic architecture under therapeutic pressure and metastatic seeding.
2. Frequent Emergence of Therapy-Resistant Subclones
Subset analyses revealed that metastatic lesions often harbor subclonal expansions of therapy-resistant populations. For example, in lung adenocarcinoma patients treated with EGFR inhibitors, metastatic biopsies showed co-occurrence of EGFR T790M and MET amplification, reflecting dual mechanisms of resistance. Similarly, in breast cancer, ESR1 mutations—rare in primaries—surfaced in metastatic biopsies following prolonged aromatase inhibitor therapy. These findings underscore the dynamic interplay between CNA evolution and clonal selection under systemic treatment.
3. Cross-Cancer Patterns of Whole-Genome Doubling
Nearly one-third of all metastatic samples bore evidence of WGD—regardless of tumor type. This pan-cancer phenomenon suggests that WGD is a generalized adaptive strategy, not confined to a specific lineage. WGD frequency was highest in late-stage epithelial tumors, including triple-negative breast cancer and pancreatic ductal adenocarcinoma, both known for genomic chaos and dismal prognoses.
4. Differential CNA Signatures by Organ Site
Metastases to different organs exhibited characteristic CNA profiles. Liver metastases frequently gained chromosome 8q (harboring MYC), lung metastases often displayed chromosome 5p amplifications (including TERT), and bone metastases—especially in prostate cancer—were enriched for 8q and 16q losses. These site-specific CNA patterns align with known metastatic tropisms and may guide organ-tailored therapies in the future.
Translational Impact and Future Directions
Incorporating CNA Profiling into Clinical Practice
As sequencing costs continue to fall, comprehensive CNA analysis can be integrated into routine clinical workflows—especially for patients with advanced disease undergoing metastatic biopsy. Prospective clinical trials should stratify participants not only by mutational status (e.g., KRAS, BRCA) but also by CNA burden and WGD status. Doing so may reveal whether high-CNA patients benefit preferentially from DNA repair inhibitors, experimental aneuploidy-targeting agents, or combination immunotherapies designed to overcome immune evasion.
Target Discovery: Exploiting Genomic Instability
The study’s identification of common CNA events suggests new avenues for drug discovery. Genes recurrently amplified in metastases—for instance, CCNE1 (cyclin E1) or RNA Polymerase I subunits on chromosome 8q—could represent vulnerabilities. Similarly, recurrent deletions of tumor suppressors—such as STK11 on 19p—may reveal synthetic lethality opportunities. By constructing “CNA dependency maps,” researchers can prioritize kinases or metabolic enzymes that become essential in the aneuploid state.
READ MORE: Exercise ‘Better Than Drugs’ to Prevent Cancer Recurrence, Landmark Trial Finds
Refining Immunotherapy Approaches
Given that a high CNA burden correlates with immunotherapy resistance, trials could evaluate whether “priming” with agents that reduce aneuploidy—such as low-dose DNA-damaging drugs or epigenetic modulators—before checkpoint blockade improves responses. Alternatively, bispecific antibodies targeting both immune checkpoints and CNA-driven immunosuppressive pathways (e.g., IDO, arginase) might reawaken anti-tumor immunity in metastatic settings.
Liquid Biopsy for Monitoring Genomic Evolution
The dynamic CNA landscape in metastasis underscores the need for noninvasive monitoring methods. Circulating tumor DNA (ctDNA) assays that quantify genome-wide copy-number changes could provide a real-time readout of metastatic progression and treatment resistance. Early detection of emergent CNAs—such as amplification of MET or ERBB2—may guide therapeutic switches before clinical relapse. Pilot studies using longitudinal ctDNA CNA profiling have shown promise in tracking WGD and aneuploidy, suggesting a feasible path to routine implementation.
Unanswered Questions and Longitudinal Studies
While CNAs emerged as the dominant genomic hallmark of metastases in this study, several questions remain:
- Temporal Ordering: At what precise moment during the metastatic cascade do CNAs arise? Single-cell sequencing of circulating tumor cells (CTCs) and micrometastases could address whether WGD often precedes dissemination or occurs post-seeding.
- Microenvironmental Pressures: To what extent do interactions with new stromal niches—such as lung, liver, or bone microenvironments—drive CNA selection? Co-culture experiments with patient-derived tumor organoids and organ-specific stromal cells could shed light on microenvironment-induced genomic instability.
- Non-Genomic Adaptations: How do epigenetic changes, metabolic rewiring, and noncoding RNAs interplay with CNAs to establish metastatic competence? Multi-omics studies combining methylation profiling, proteomics, and single-cell RNA sequencing will be essential.
- CNA Heterogeneity Within Metastases: Do all cells within a single metastatic lesion share similar CNA profiles, or do CNA subclones coexist? Spatial transcriptomic and DNA-FISH analyses could delineate the intrametastatic architecture.
Conclusion: Toward Smarter, More Adaptive Cancer Therapies
The Weill Cornell Medicine and MSK collaboration offers a paradigm shift: metastatic progression in solid tumors is driven less by the accumulation of novel point mutations and more by large-scale chromosomal upheavals. By emphasizing copy-number alterations—particularly whole-genome doubling—this research elucidates how metastatic cells maximize genetic diversity while minimizing immune detection.
Clinicians and translational scientists must now integrate CNA profiling into precision oncology frameworks. Doing so will allow personalized treatment plans that anticipate metastatic trajectories, exploit DNA repair vulnerabilities in highly aneuploid cells, and adapt immunotherapy strategies to surmount CNA-driven immune evasion. As our genomic tools become ever more sophisticated, the ability to track and target the CNA landscape in real time promises to revolutionize care for patients with advanced cancer—transforming metastasis from a largely fatal event into a manageable, treatable condition.