Since the COVID-19 pandemic began, cervical cancer screening rates in England have fallen from 72.2 percent in 2020 to 68.4 percent in 2024, NHS England data shows. A recent YouGov survey of 3,000 eligible individuals—commissioned by Cancer Research UK—finds that 30 percent of respondents are now overdue for their routine cervical screening. Experts warn that this sustained decline poses a serious obstacle to the NHS’s pledge to eliminate cervical cancer by 2040.
Key Barriers to Screening Uptake
Pain and Discomfort
• 42 percent of those overdue report having found previous screenings painful.
• Some clinicians say that discomfort often stems from ill-fitting speculum sizes or rushed appointments.
Gender of the Practitioner
• 40 percent of overdue respondents say they would prefer a female practitioner.
• NHS trusts are being urged to accommodate gender preferences by expanding clinic choices.
Embarrassment and Misconceptions
• 19 percent of those who skipped screening report feeling “too embarrassed” to attend.
• 16 percent believed screening was unnecessary in the absence of symptoms.
“These figures tell us that misunderstandings remain deeply rooted,” says Fiona Osgun, Cancer Research UK’s Head of Health Information. “Even a successful programme can lose momentum if we do not address both the practical and psychological barriers people face.”
Regional Variation in HPV Vaccine Uptake
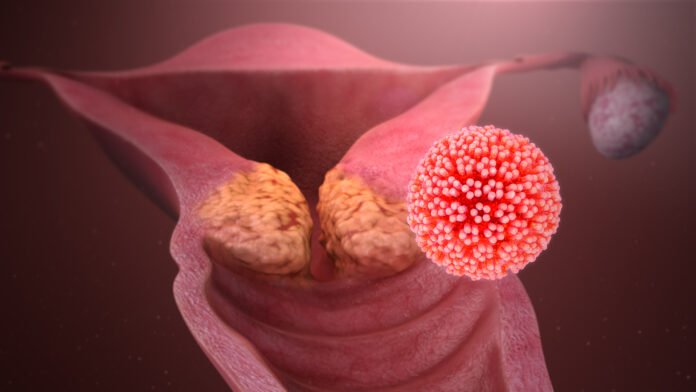
Uptake of the human papillomavirus (HPV) vaccine—an effective primary prevention for cervical cancer—also varies widely by region, according to the UK Health Security Agency:
• London girls aged in school Year 10: 64.9 percent vaccinated
• South East girls aged in Year 10: 82.7 percent vaccinated
• London boys in Year 10: 58.9 percent vaccinated
• South East boys in Year 10: 77.3 percent vaccinated
“Low vaccine uptake in London leaves large urban cohorts at excess risk,” warns Dr. Amanda Doyle, NHS England’s National Director for Primary Care and Community Services. “We must target outreach efforts and dispel myths that fuel hesitancy.”
Impact on Incidence and Mortality
Each year in the UK:
• 3,200 new cervical cancer diagnoses
• 850 deaths from cervical cancer
Cervical cancer ranks as the 14th most common cancer affecting women in Britain, with the highest incidence in those aged 30 to 34. Globally, it is the fourth most common cancer in women, accounting for about 660,000 new cases and 350,000 deaths annually, according to the World Health Organization.
Revised Screening Intervals for Low-Risk Individuals
In June 2025, NHS England updated its guidelines for people aged 25 to 49 who test negative for high-risk HPV strains. These individuals—at very low risk of developing cervical cancer—will now be invited for screening every five years instead of three. “Extending intervals for low-risk groups allows us to concentrate resources on those most in need,” says Dr. Doyle.
Calls for Greater Flexibility and Support
Appointment Accessibility
• Offering early-morning, evening, and weekend clinic slots can help those juggling work or family commitments.
• Extended reminder systems—via text, email, or phone—have been shown to boost attendance.
Comfort Measures
• Double appointments or extended slots reduce the sense of rush.
• Speculum choice and lubrication options can minimize discomfort.
Community Outreach and Education
• Peer-led workshops and educational campaigns in schools and local centres can improve awareness.
• Targeted interventions in areas with low HPV vaccination can prevent future cancer cases.
Next Steps for Policymakers
Achieving the 2040 elimination target will require a two-pronged approach: bolstering both primary prevention (HPV vaccination) and secondary prevention (screening). “Policymakers must invest in capacity—more clinics, more trained staff, and expanded community outreach,” says Osgun. “We also need better data systems to identify and support under-screened groups in real time.”
Long-Term Outlook
While the recent decline in screening rates is concerning, experts believe it is reversible. “Screening programmes historically recover after dips, provided there is sustained effort and innovation,” notes Dr. Doyle. “By addressing barriers head-on and tailoring services to people’s needs, we can turn the tide and stay on track to wipe out cervical cancer by 2040.”
Cervical screening remains the cornerstone of early detection, capable of identifying pre-cancerous changes long before symptoms arise. Paired with wide HPV vaccine coverage, it offers the most effective strategy yet to consign cervical cancer to history. The next two years will prove critical: every screening and every vaccine counts toward safeguarding future generations.